In Sweden, around 1,000 children and an equal number of adults develop type 1 diabetes each year. The disease has major consequences for the families affected. Children with type 1 diabetes need help keeping track of their blood glucose and taking insulin injections. Teenagers and adults need to take great personal responsibility for their disease. Type 1 diabetes may lead to complications in both the short and long term. Early detection can delay complications, and above all, prevent severe illness.
"Early diagnosis means a lot to reduce the risk of complications. With the help of screening, we can catch children at an early stage, before they become very ill," says Åke Lernmark, senior professor of experimental diabetes at Lund University.
He is active within EXODIAB, which is a strategic research area in diabetes at Lund University. During a more than 50-year career that includes research in Sweden, the United States and Denmark, he has been driven by the same question – what causes some children to develop type 1 diabetes?
Engaged in method development
His many years of studies of diabetes-related autoantibodies have contributed to increased knowledge about type 1 diabetes so that it may become possible to start screening children for the disease. Diabetes-related autoantibodies can be used to identify people who are at risk of developing type 1 diabetes.
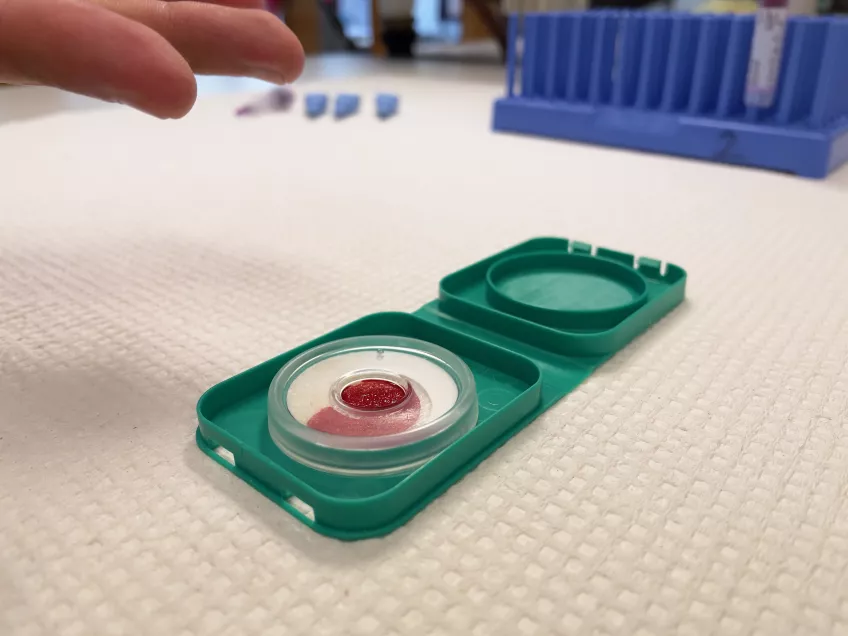
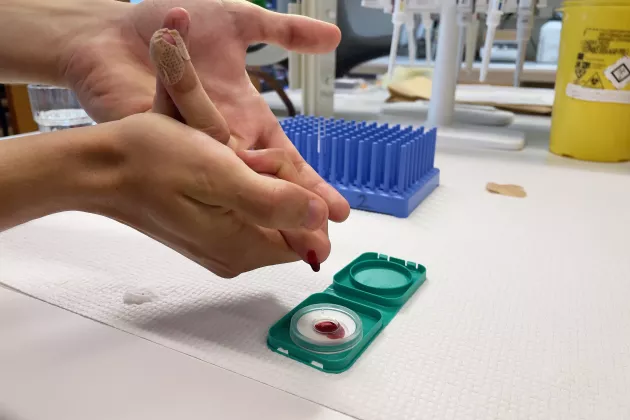
Åke Lernmark has, for example, developed a method called RBA (radiobinding assay) to measure the presence of diabetes-related autoantibodies in the blood. It has become an international standard method, used worldwide. In the years since the RBA was developed, new methods have emerged that can be used to screen for type 1 diabetes more effectively. One such example is the ADAP method (antibody detection by agglutination-PCR), which has been developed by researchers in the United States. The advantage of this method is that the measurements can be automated instead of being done manually. Åke Lernmark recently coordinated a study comparing the two methods which showed that the new method was as good or better than the RBA method in defining which children are at risk of developing type 1 diabetes.
"Developing optimal screening methods that can be used in healthcare is absolutely crucial to getting a national screening programme in place," says Åke Lernmark.
Knowledge of how families react
He has also been instrumental in carrying out the international TEDDY study, which included more than 8,000 children in Sweden, Finland, the United States and Germany with an increased hereditary risk of developing the disease. The study, which started in 2004, has followed the children up to the age of 15, and sampling is now being completed. The TEDDY study has resulted in many important lessons, not least in terms of how parents act when they are informed that their child has developed diabetes-related autoantibodies.
"What happens when parents learn that there is an autoantibody is that they read up on the disease. Everyone does something to delay their child developing diabetes, such as changing the diet for example. Above all, they pay attention to early symptoms, something that can avoid hospitalisation and serious illness. This bodes well for a future screening programme," says Åke Lernmark.
He is also involved in collaborations that investigate opportunities to introduce screening for type 1 diabetes in Sweden. An example is his work within an innovation environment called ASSET, which includes various universities, companies, hospitals and the National Diabetes Registry. One of the aims of ASSET is to develop and evaluate new algorithms that can be used to assess the individual risk of developing type 1 diabetes and the likelihood of responding to different treatments. The data that will initially be used to build the algorithms comes from, among other data sources, the TEDDY study.
Treatments mean new possibilities
ASSET participants also lead workshops for authorities and other actors to discuss issues related to screening for type 1 diabetes. The National Board of Health and Welfare has many criteria that need to be met in order for a national screening programme in type 1 diabetes to become a reality in Sweden. The most important criterion is that there must be a treatment that either prevents or delays the disease. In the United States, the drug Teplizumab, which can slow the progression of type 1 diabetes, has been approved for use.
"If the drug Teplizumab is approved in Sweden, it is important that we have a readiness to start screening for the disease," says Åke Lernmark.
Åke Lernmark and the other participants in the innovation environment are now developing proposals for how a screening programme that meets the National Board of Health and Welfare's criteria could look like. One suggestion is that all children should be tested on two occasions – once when they are four years old and once when they are between seven and eight years old. Then many children who are at risk of getting the disease can be followed up to ensure that they receive care at an early stage, and thus prevent them from becoming seriously ill.
Collaboration is important
It is also important to create the right organisational, financial and legal conditions because major changes in the healthcare system will be required if a national screening programme is to work. The academic think tank Leading Health Care is one of the participants in ASSET. The task of the think tank is to create a dialogue with the organisations and actors that are affected, for example regions, patient organisations and authorities.
"We work with the systems perspective, where we examine how a screening programme could be implemented in healthcare. There are many challenges that must be solved, linked to capacity and infrastructure, costs for screening, and what knowledge-raising efforts may be needed," says Hans Winberg, secretary general of Leading Health Care.
The think tank works to influence the development of health care in new directions. Åke Lernmark and other researchers within the strong research area EXODIAB contribute important knowledge, as do other universities, patient organisations and companies.
"If we are to bring this to fruition, we must cooperate widely and involve the healthcare system, companies, researchers and patient organisations. If we go further in our process, I hope that we can contribute with input into how this can be implemented and organised. It's a learning experience for us too," says Hans Winberg.
Reduced suffering
Åke Lernmark thinks a lot about the importance of a national screening programme for people who develop type 1 diabetes. Even though Sweden has very good diabetes care, many suffer from complications linked to the kidneys, heart, feet and eyes.
"Type 1 diabetes costs so much in both suffering and resources. If we can delay the disease, it can hopefully lead to fewer complications. If we can test all children, we will also have the opportunity to do more research on what actually causes the disease."
He also reflects on his own and others' progress in diabetes research in recent years, without which screening would not have been possible. The work within EXODIAB has given him the right support and network to make a difference.
"As a researcher, you are never alone. You seek out researchers and other actors who are pulling in the same direction. Now that we have research and collaborations that can enable screening, I believe we are on the way to reaching a new milestone in terms of type 1 diabetes."